Hello and welcome to the CSRA mnd computer-based training for New York State Medicaid providers. This is the first video in our new provider new biller series of tutorials. The purpose of this session is to familiarize providers with the roles and responsibilities of the Medicaid partners. The Medicaid partners include the New York State Department of Health, CSR amme County Department of Social Services, Office of the Medicaid Inspector General, New York State of Health managed care plans, and you, the providers. The New York State Department of Health is responsible for Medicaid policy, procedure codes, required claim documentation, setting fees and rates, prior approvals, monitoring of Fraud and Abuse, over two-year claim procedures, and provider enrollment. The website for the New York State Department of Health is WWF NY govt. In-state providers can reach the New York State Department of Health at 834 to three zero zero five, and out-of-state providers can call the State Department of Health at five one eight four seven four three five seven five. CS REM nd, as the fiscal agent for New York state's Medicaid program, is responsible for processing your Medicaid claims, maintaining provider manuals on the amenity website, remittance statements, and checks, electronic funds transfer, billing inquiries and guidelines, Medicaid provider training, issuing paper claim forms (not including the ubo for electronic transmitter ID numbers or Ethan's heat cases), the electronic provider-assisted claim entry system, and provider enrollment for fee-for-service providers. Stance ramm me is also responsible for meds the Medicaid eligibility verification, as well as the VeriFone POS terminal for checking eligibility, the drug utilization review program (do you are), and the dispensing validation system (DVS). Contact information for CSR AM Edney - the website is WWE M et NY org, and amenity provider services can be reached at 834 three...
Award-winning PDF software





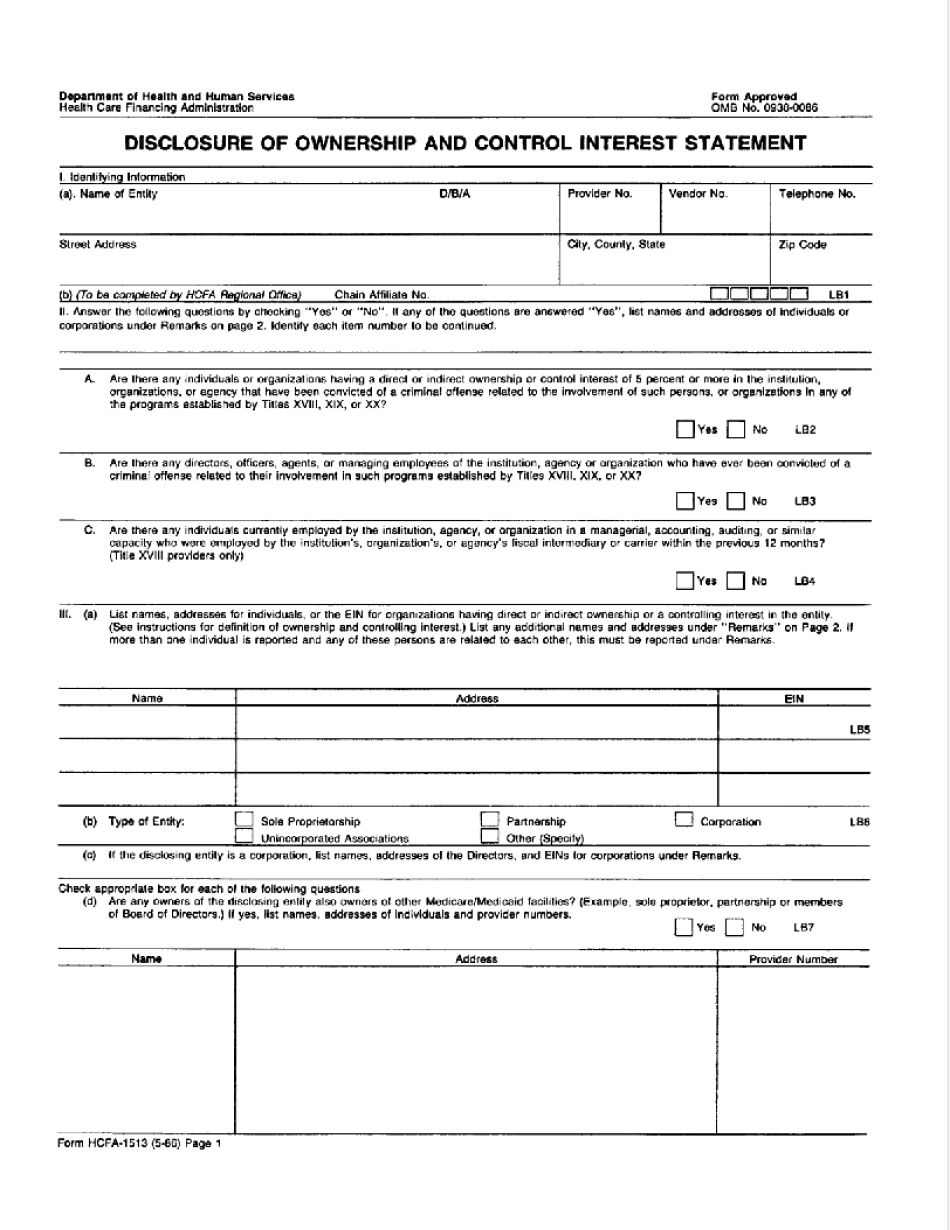
Kentucky medicaid disclosure of ownership Form: What You Should Know
State Requirements Pursuant to section 17-21-23(1), the Secretary of the Department shall determine the size of provider networks for Medicaid providers, and the Secretary of Insurance shall ensure that all Medicaid providers, with respect to which the applicant seeking a provider enrollment has submitted an appropriate notice to the Secretary of the Department, comply with the requirements of this chapter. SECTION 23. No Medicaid Provider shall receive, or contract for, any fee, amount, benefit, or other thing of value from a managed care organization for the purpose of, or as compensation for, the delivery of any health care services or services in connection with the provider's ability to accept claims from a particular patient, including but not limited to, reimbursement for services that are billed by a member health care plan, or that are billed through a third-party reimbursement service. The Secretary of the Department shall develop, implement, and update a procedure for verifying, among other things, that each Medicaid provider, when accepting the claims of a particular resident, is acting exclusively in that patient's best interest through the provision of quality care with respect to medical necessity, and in accordance with the standards described below, and providing notice of this requirement to each Medicare patient who undergoes any service or a hearing or rehabilitation examination for which an approved Medicare health care payment was made to a Medicaid provider for the provider's services, and to each member health care plan, upon becoming eligible for Medicare, in the case of members. The notification shall be sent to the last known address of the Medicaid provider and in any event shall be sent, in the case of a member, not later than 10 days prior to any scheduled hearing or rehabilitation. After receiving this notification, the Medicare beneficiary's plan shall provide a separate notice to Medicare and the health plan or health plan administrator of the member. Each Medicaid provider, when accepting an action that is billed by a member health care plan, or that is billed through a third-party reimbursement service, shall: 1. Verify that the health care service was medically necessary for the patient, the beneficiary's medical condition and needs, and for appropriate treatment of the health care service or service; 2. Verify that the provider, in his or her reasonable professional judgment, was unable to provide the requested health care service in accordance with accepted medical standards; 3.
online solutions help you to manage your record administration along with raise the efficiency of the workflows. Stick to the fast guide to do HCFa-1513, steer clear of blunders along with furnish it in a timely manner:
How to complete any HCFa-1513 online: - On the site with all the document, click on Begin immediately along with complete for the editor.
- Use your indications to submit established track record areas.
- Add your own info and speak to data.
- Make sure that you enter correct details and numbers throughout suitable areas.
- Very carefully confirm the content of the form as well as grammar along with punctuational.
- Navigate to Support area when you have questions or perhaps handle our assistance team.
- Place an electronic digital unique in your HCFa-1513 by using Sign Device.
- After the form is fully gone, media Completed.
- Deliver the particular prepared document by way of electronic mail or facsimile, art print it out or perhaps reduce the gadget.
PDF editor permits you to help make changes to your HCFa-1513 from the internet connected gadget, personalize it based on your requirements, indicator this in electronic format and also disperse differently.
Video instructions and help with filling out and completing Kentucky Medicaid Disclosure Of Ownership Form